Ultrasonography of the Lymph Nodes
Check out this article below: Ultrasonography of Lymph Nodes
Assessment of the lymph nodes should form part of a routine abdominal ultrasound examination.
The abdomen contains many lymph nodes. Though many lymph nodes are not easily visualised when normal, there are some groups that are routinely seen on ultrasound examination, and it is important to be able to recognise them, as well as be able to identify enlargement and change in lymph node appearance in cases of pathology.
Normal anatomy
.jpg)
The abdominal lymph nodes are divided into the visceral group (including the hepatic, splenic, gastric, pancreaticoduodenal, jejunal, and colic lymph nodes) and the parietal group (including the lumbar aortic, renal, medial iliac, internal iliac, and sacral lymph nodes).
A schematic illustration of the locations of the abdominal lymph nodes. Left – the visceral group: 1. Hepatic 2. Gastric 3. Pancreaticoduodenal 4. Splenic 5. Colic 6. Jejunal. Right – the parietal group: 7. Renal 8. Lumbar aortic 9. Medial iliac 10. Internal iliac (hypogastric) 11. Sacral.
When patients present with pathological changes and/or when changes in lymph nodes are seen, it can be useful to consider the anatomic areas drained by each group.
| Lymph Nodes | Draining area includes |
| Lumbar aortic, Renal | Diaphragm, caudal ribs, lumbar vertebrae, lumbar muscles, peritoneum, liver, kidneys, adrenal glands |
| Splenic, gastric, hepatic, pancreatic | Spleen, stomach, oesophagus, duodenum, liver, pancreas, peritoneum |
| Jejunal, colic | Jejunum, ileum, pancreas, caecum, colon, rectum |
| Medial iliac, internal iliac, sacral | Colon, rectum, caudal urogenital system, hindlimbs |
Examination technique
The highest frequency setting that gives adequate depth of penetration to view the area of the lymph nodes should be used. In some patients, a frequency of 7.5Mhz is adequate. However, higher frequencies (8-15Mhz) will improve image resolution and can be utilised in smaller patients. Either a micro-convex or linear transducer can be used for the examination. Linear transducers are capable of higher frequency settings and are ideal for smaller patients. However, their larger footprint makes them harder to manoeuvre around the body. In comparison, micro-convex transducers produce a lower frequency range though their smaller, curved surface make them ideal in larger patients and for imaging using the intercostal spaces.
Lymph nodes which are routinely identified include the jejunal and medial iliac nodes.
Jejunal Lymph Nodes
The jejunal lymph nodes are located adjacent to the cranial mesenteric artery and vein in the middle third of the right abdomen. With the patient in left or right lateral recumbency, the lymph nodes and/or adjacent vessels may be visualised when performing a “castle” or “grid” pattern scan to view and assess the small intestine.
By orientating the transducer to view the vessels in a longitudinal plane, small fanning motions can be made to either side of the vessel to identify the lymph nodes. Colour Doppler mode can be used to differentiate the hypoechoic lymph nodes from neighbouring hypo- / anechoic vascular structures.
Medial Iliac Lymph Nodes
The medial iliac lymph nodes are located adjacent to the aorta, between the deep circumflex arteries and the internal iliac arteries. There is usually one lymph node on each side of the aorta, however, more can be present.
With the patient in right or left lateral recumbency, the aorta can be identified in the dorsal abdomen, ventral to the vertebral column and to the left of the midline. With the transducer marker orientated cranially, a dorsal or sagittal plane view of the aorta can be achieved. The transducer can then be slid to follow the aorta caudally to the level of the aortic bifurcation (trifurcation) – the point at which the external iliac arteries branch from the aorta. Here, the transducer can be fanned dorsally and ventrally to visualise the area of the medial iliac lymph nodes.
Normal appearance
Normal lymph nodes appear homogenous and uniformly hypoechoic. They have an oval – fusiform shape and can vary in thickness and length. Occasionally, a hyperechoic linear hilus can be seen1.
In comparison to adult dogs, the jejunal lymph nodes of younger dogs can appear larger, more heterogenous, and with a greater variety in shape2,3.
.jpg)
Jejunal Lymph Node. In this sagittal oblique plane image of the mid right abdomen of a normal dog, part of the jejunal lymph node can be seen (red arrow) adjacent to the cranial mesenteric artery (yellow arrow).
As the jejunal lymph nodes vary in shape and can be up to 6cm in length, reference ranges for size are based on short axis measurements:
With the lymph node in a transverse plane, measure the maximum width and the maximum height.
Normal height: median 0.39cm (range 0.16-0.82cm)4
Normal width: median 0.75cm (range 0.26-1.5cm)4
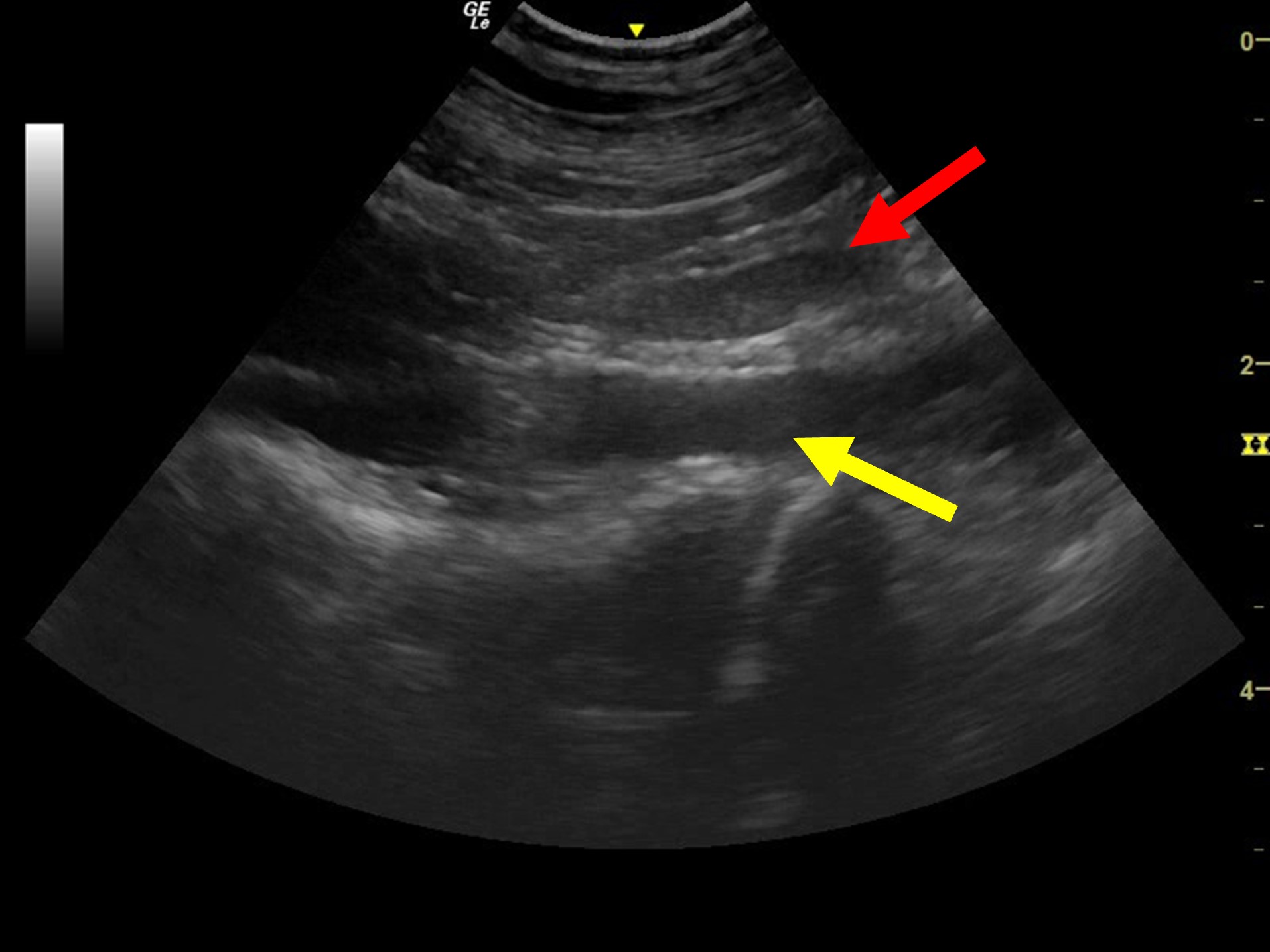
Medial Iliac Lymph Node. In this dorsal plane image of the caudodorsal abdomen of a normal dog, a medial iliac lymph node can be seen in the near field (red arrow) adjacent to the right external iliac artery (yellow arrow).
The medial iliac lymph nodes can be measured by recording the width at the maximum diameter of the lymph node:
Approximate average width: 0.60 cm (reported range depending on dog weight: 0.37-0.89cm)5
Ultrasonographic appearance of lymph node pathology
Lymphadenopathy can be caused by reactivity, and primary or metastatic neoplasia. It is important to recognise that there is an overlap between the changes seen in benign and malignant pathology, and that aspiration or biopsy is necessary for a definitive diagnosis. Reactive hyperplasia reflects activity of the node as part of a local or generalised immune response and can be caused by a wide range of conditions.
In comparison to normal lymph nodes, neoplastic lymph nodes can appear larger, more rounded, irregular in shape, hypoechoic, heterogenous, with reduced hilar tissue definition, and altered vascularisation6.
As neoplastic lymph nodes become more rounded in comparison to normal lymph nodes, the ratio of short:long axis measurement has been used as an indicator of malignancy. In one study, the lymph nodes of dogs affected by lymphoma had short:long axis of >0.7, whereas normal or reactive nodes had a short:long axis of <0.67. Another study proposed a short:long axis cut-off of >0.48 for malignant nodes, and ≤0.48 for reactive nodes8. However, the short:long axis may be of limited use in some lymph nodes, such as the jejunal nodes, which tend to be longer and curved, making it difficult to accurately measure the length.
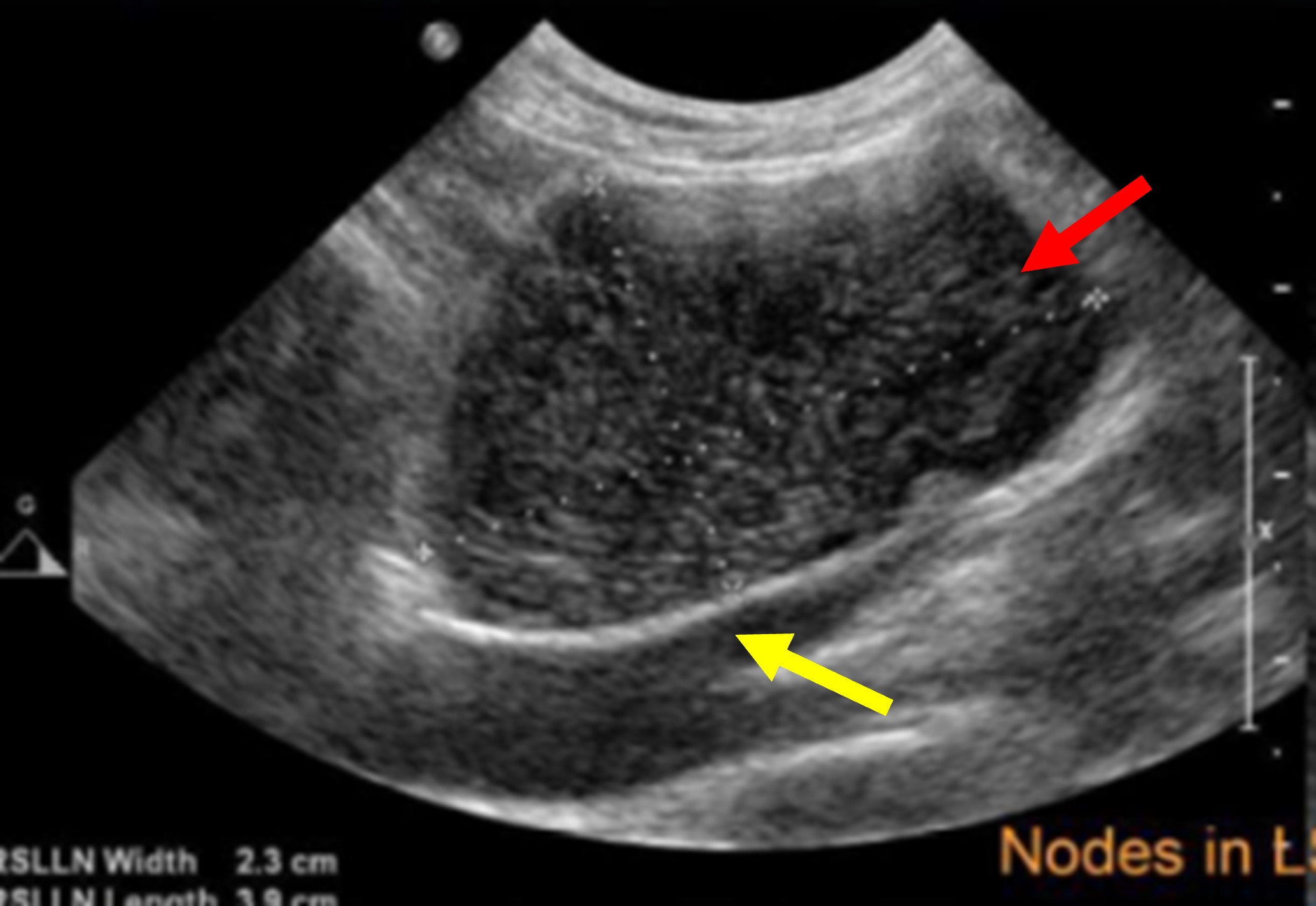
Neoplastic Medial Iliac Lymph Node in a Dog. In this dorsal plane image, an abnormal medial iliac lymph node can be seen (red arrow). The node appears hypoechoic, heterogenous, enlarged with a more rounded shape, with a short:long axis of 0.6. The adjacent external iliac artery is visible in the far field (yellow arrow).
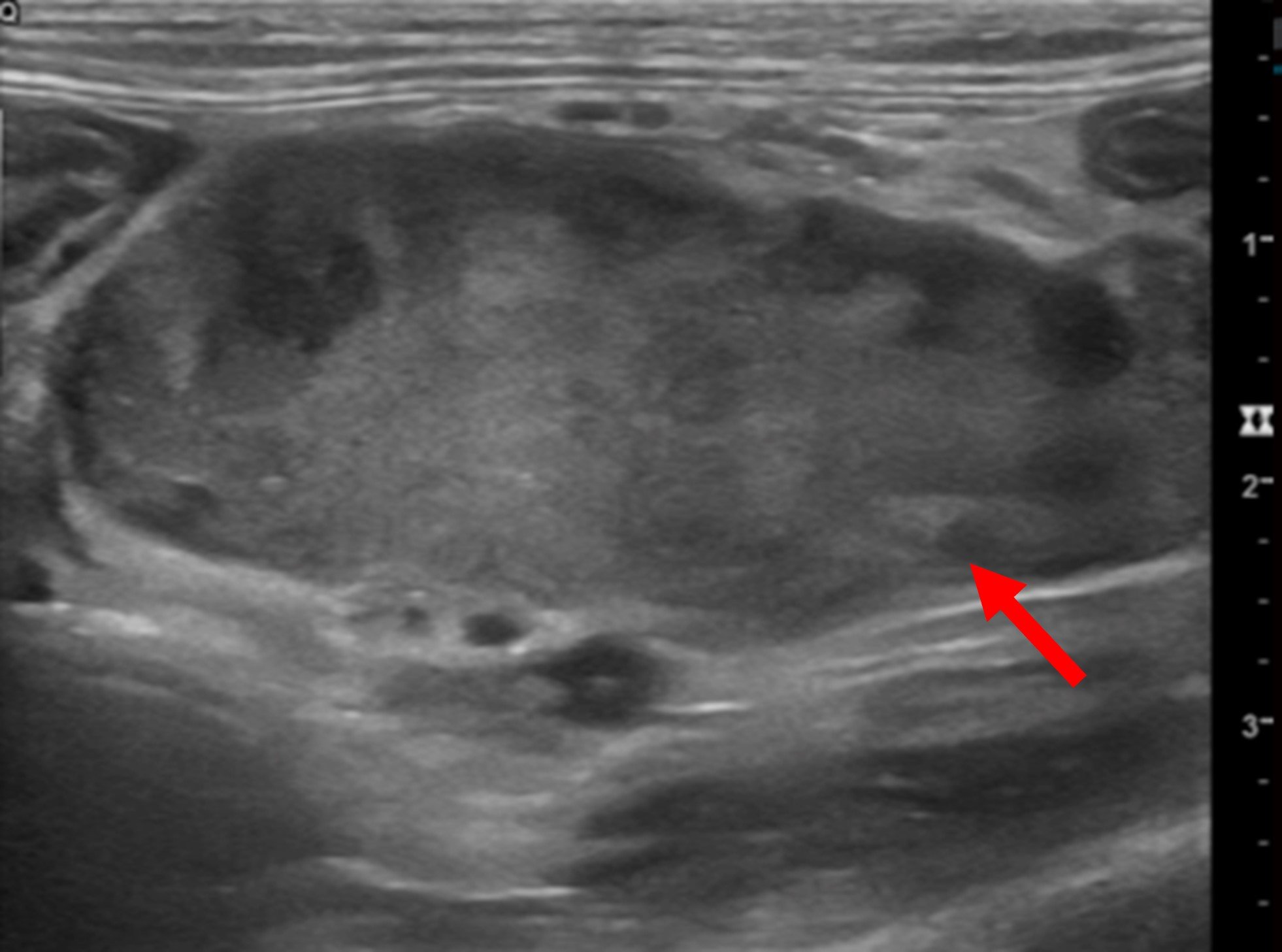
Neoplastic Jejunal Lymph Node. In this sagittal oblique plane image of the mid abdomen, an enlarged jejunal lymph node can be seen (red arrow). The node is heterogenous with multiple peripheral hypoechoic areas and is rounded with irregular contours.
Sampling considerations
Ultrasound can be used to guide needle placement for fine needle aspiration of the abdominal lymph nodes. Additionally, Doppler ultrasound can be used to document and avoid local vascular structures.
Generally, a 22 – 25-gauge needle is used with needle length dictated by the depth of the node to be sampled. A minimum of three non-aspiration technique samples are recommended for each lymph node sampled9.
References
- Kinns J. (2012) Abdomen. In: BSAVA Manual of Canine and Feline Ultrasonography. Eds. Barr F., Gaschen L. Gloucestershire: British Small Animal Veterinary Association, pp 72–84.
- Krol L., O’Brien R. (2012) Ultrasonographic assessment of abdominal lymph nodes in puppies. Veterinary Radiology & Ultrasound 53: 455-458.
- Stander N., Wagner W.M., Goddard A. Kirberger R.M. (2010) Normal Canine Pediatric Gastrointestinal Ultrasonography. Veterinary Radiology & Ultrasound 51: 75-78.
- Agthe P., Caine A., Posch B., Herrtage M. (2009) Ultrasonographic appearance of jejunal lymph nodes in dogs without clinical signs of gastrointestinal disease. Veterinary Radiology & Ultrasound 50:195-200.
- Mayer M.N., Lawson J.A., Silver T.I. (2010) Sonographic characteristics of presumptively normal canine medial iliac and superficial inguinal lymph nodes. Veterinary Radiology & Ultrasound 51:638-641.
- De Swarte M., Alexander K., Rannou B., D’anjou, M.A., Blond I., Beauchamp, G. (2011) Comparison of sonographic features of benign and neoplastic deep lymph nodes in dogs. Veterinary Radiology & Ultrasound 52: 451-456.
- Nyman H.T., Kristensen A.T., Skovgaard I.M. McEvoy F.J. (2005), Characterization of normal and abnormal canine superficial lymph nodes using grey-scale B-mode, colour flow mapping, power, and spectral doppler ultrasonography: a multivariate study. Veterinary Radiology & Ultrasound 46: 404-441.
- Belotta A.F., Gomes M.C., Rocha N.S., Melchert A., Giuffrida R., Silva J.P., Mamprim M.J. (2019) Sonography and sonoelastography in the detection of malignancy in superficial lymph nodes of dogs. Journal of Veterinary Internal Medicine 33: 1403–1413.
- Liffman R., Courtman N. (2017) Fine needle aspiration of abdominal organs: a review of current recommendations for achieving a diagnostic sample. Journal of Small Animal Practice 58: 599–609.
Further Reading
d’Anjou M.A., Carmel E.N. (2015) Abdominal Cavity, Lymph Nodes, and Great Vessels, In: Atlas of Small Animal Ultrasonography 2nd edn., Eds: Penninck D., d’Anjou M.A., John Wiley & Sons, Chichester, pp 455-479.
Nyman H.T., O’Brien R.T., (2007) The sonographic evaluation of lymph nodes, Clinical Techniques in Small Animal Practice 22: 128-137.
Widmer W.R., Mattoon J.S., Nyland T.G. (2015) Peritoneal Fluid, Lymph Nodes, Masses, Peritoneal Cavity, Great Vessel Thrombosis, and Focused Examinations, In: Small Animal Diagnostic Ultrasound 3rd edn., Eds. Mattoon J.S., Nyland T.G., Elsevier, St. Louis, pp 501-516.
View our Ultrasound Products >>
We hope you enjoyed this blog post!
Don’t forget to share! 👇


