Journal Club – Vertebral Left Atrial Score (VLAS)
Journal Club – Summary
This month’s Journal Club assesses the literature associated with the measurement ‘Vertebral Left Atrial Score (VLAS)’
Vertebral Left Atrial Score (VLAS)
UK visitors only – After watching the video, a pop up will appear which will allow you to enter your details to receive your CPD certificate.
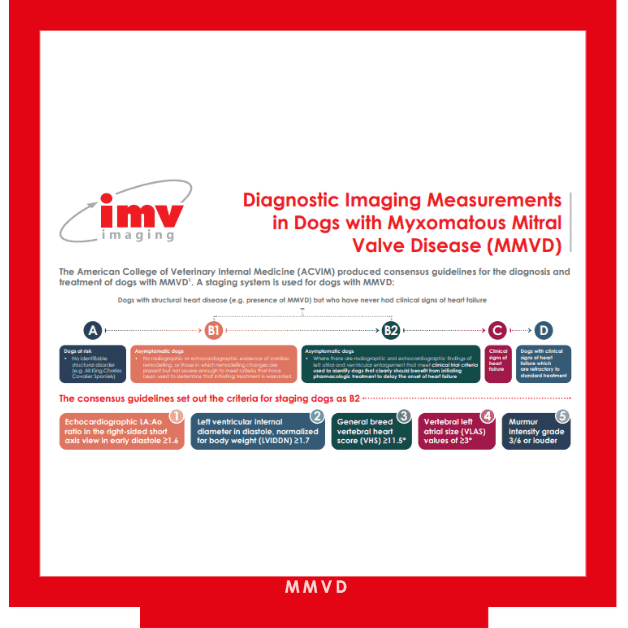
In 2019 the American College of Veterinary Internal Medicine (ACVIM) produced a consensus statement on the diagnosis and management of myxomatous mitral valve disease (MMVD) in dogs:
- Keene B.W., Atkins C.E., Bonagura J.D., Fox P.R., Häggström J., Luis Fuentes V., Oyama M.A., Rush J.E. Stepien R., Uechi M. (2019) ACVIM consensus guidelines for the diagnosis and treatment of myxomatous mitral valve disease in dogs. Journal of Veterinary Internal Medicine 33: 1127-1140
The consensus utilises a grading system for dogs with MMVD. Within this system, dogs with structural heart disease but without clinical signs of heart failure are categorised as stage B. Stage B is then further categorised as B1 or B2; stage B2 is when radiographic and echocardiographic findings of left atrial and ventricular enlargement are present. Identifying dogs that can be categorised as stage B2 is important as clinical trials have shown that at this stage, they benefit from starting treatment to delay the onset of heart failure1.
The 2019 consensus states that a radiographic measurement, Vertebral Left Atrial Score (VLAS), could potentially be of value in identifying dogs who meet the criteria for stage B2 MMVD.
This month’s Journal Club assesses the literature associated with this measurement.
Three recent journal articles were examined:
- Malcolm E.L., Visser L.C., Philips K.L., Johnson L.R. (2018) Diagnostic value of vertebral left atrial size as determined from thoracic radiographs for assessment of left atrial size in dogs with myxomatous mitral valve disease. Journal of the American Veterinary Medical Association 253: 1038 -1045
- Vezzosi T., Puccinelli C., Tognetti R., Pelligra T., Citi S. (2020) Radiographic vertebral left atrial size: A reference interval study in healthy adult dogs. Veterinary Radiology and Ultrasound; 1-5
- Stepien R.L., Rak M.B., Blume L. M. (2020) Use of radiographic measurements to diagnose stage B2 preclinical myxomatous mitral valve disease in dogs. Journal of the American Veterinary Medical Association 256: 1129 – 1136
Paper 1 described VLAS and investigated the value of the measurement in predicting left atrial (LA) enlargement in dogs with MMVD. The study investigated dogs with MMVD that had had 3 view thoracic radiographs 24 hours prior to or following an echocardiographic examination.
VLAS was measured on the right and left lateral projections. The VLAS measurement is performed as below:
- A line is drawn from the centre of the most ventral aspect of the carina to the most caudal aspect of the left atrium where it intersected with the dorsal border of the caudal vena cava
- The carina was defined as the radiolucent circular or ovoid structure within the trachea that represented the bifurcation of the left and right mainstem bronchi
- A second line that was equal in length to the first was drawn beginning at the cranial edge of T4 and extending caudally just ventral and parallel to the vertebral canal
- The VLAS was defined as the length of the second line expressed in vertebral body units to the nearest 0.1 vertebra
The same investigator also performed echocardiographic measurements to assess LA size using Left atria to aortic ratios performed on right parasternal long and short axis views (LA:AoSx and LA:AoLx respectively).
The study population was composed of 103 dogs which were graded based on the ACVIM consensus.
The study found that VLAS as determined from right lateral thoracic radiographs did not differ significantly from the VLAS as determined from left lateral thoracic radiographs and that the intraobserver and interobserver correlations for VLAS were high regardless of the lateral thoracic image used for measurement. There was a significant positive correlation between VLAS and both LA:AoSx and LA:AoLx, and VLAS cutoffs of 2.3 to 2.5 vertebrae were associated with an LA:AoSx ≥ 1.6 and LA:AoLx ≥ 2.6. The study suggested a VLAS ≥ 2.3 vertebrae can be used as a radiographic indicator of LA enlargement.
The study had some limitations. The control group only composed of 15 dogs and some of the dogs which were more severely affected with congestive heart failure secondary to MMVD had had treatment with medication which could have affected the measurements used in the study.
The purpose of Paper 2 was to describe a reference range for VLAS in healthy dogs. The study measured VLAS as described by Paper 1 and performed the measurement on right lateral thoracic radiographs. Dogs used in the study were defined as healthy based on history, radiography and echocardiography (the dogs had a LA:AoSx ration of <1.6).
The study population was made up of 80 dogs. No effect of body weight, sex, and age on VLAS was detected based on multivariate analysis and the intraobserver and interobserver measurement agreement for VLAS was excellent. The median value of VLAS was 1.9 and the study suggested a reference range for VLAS in healthy dogs of 1.4 to 2.2.
A limitation of this study is that, like vertebral heart size, it is hypothesised that VLAS may vary due to breed variation. As a study of healthy dogs this investigation included no breeds of certain conformations.
Paper 3 investigated the usefulness of radiographic measures of the left atria and left ventricle as surrogates for echocardiographic criteria in identifying dogs with stage B2 MMVD. The measures investigated included VLAS.
The study investigated dogs diagnosed with preclinical MMVD, with heart murmurs ≥3/6 and a body weight between 4 and 15Kg. The dogs had undergone an echocardiographic exam and thoracic radiography within the same 24-hour period. Dogs in study were grouped as to whether they did (case dogs) or did not (control dogs) meet the criteria for categorisation of stage B2 MMVD (LA:AoSx ≥ 1.6 and a left ventricular internal diameter in diastole normalised for weight of ≥ 1.7 (LVIDDN)).
An independent observer reviewed the thoracic radiographs for each dog and made several measurements including VLAS. VLAS was measured using the technique described in Paper 1but they expressed the result in vertebral body units (VBU) to the nearest 0.25.
56 dogs made up the study group. Results showed that measurements pertaining to left atrial were the most accurate at identifying case dogs. Of these, VLAS was the simplest to perform in a clinical setting. A VLAS cut off for dogs meeting the criteria of stage B2 MMVD was identified as 2.5.
Intraobserver repeatability was not assessed in this study. However, the previous studies summarised would suggest repeatability is good. There was only 26 control dogs present in the study, 15 of which had discordant echocardiographic results, with either the combination of LVIDDN ≥ 1.7 and LA:Ao < 1.6 (n = 11) or the combination of LVIDDN < 1.7 and LA:Ao ≥ 1.6 (n=4). Also, VLAS was measured to the nearest 0.25 VBU which would influence the reported cut-off values and differs from the previous studies.
VLAS Summary
- As a measurement, VLAS is simple and repeatable
- Increases in VLAS correlate with increases in LA size as determined by echocardiography
- A VLAS ≥ 2.3 – 2.5 can be used as an indicator of LA enlargement. Dogs exceeding this cut off likely have haemodynamically important MMVD
- More work needs to be done on establishing a normal range and assessing breed variability
- VLAS cannot be applied to conditions other than MMVD
- Echocardiography remains the preferred method of identifying dogs with stage B2 MMVD
References
- Boswood A, Häggström J, Gordon SG, et al. (2016) Effect of Pimobendan in dogs with preclinical myxomatous mitral valve disease and cardiomegaly: the EPIC study—a randomized clinical trial. J Vet Intern Med. 30: 1765-1779.